Wednesday (7/26) morning, Chris went to see a new urologist about his kidney stones. This new urologist was surprised to see that he had done an IVP X-ray for the kidney stones. He remarked that IVPs are not very clear and insisted that Chris have a CT Scan, instead. He was also surprised at the frequency Chris has been getting the kidney stones and says that as soon as this kidney stone is treated, he's referring Chris to a nephrologist for prevention. This was a nice change from Chris' previous urologist who would use multiple treatments to break up the kidney stone and then send Chris on his way without any information on prevention. We were beginning to think that we were just a paycheck for him.
Wednesday night and Thursday morning were very painful for Chris and he wasn't able to return to work Thursday as he had planned. Thursday afternoon, he passed two rather large fragments and he felt much better. He was able to return to work Friday relatively free of pain. Unfortunately, without the pain of the kidney stones distracting him and with many offers of sympathy from co-workers, Chris felt the loss of Eric more keenly than he had been able to before.
Monday, July 31, 2006
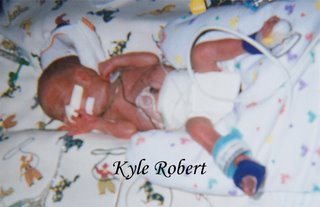
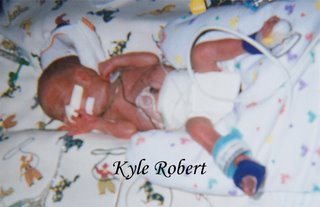
Update on Kyle
Kyle is still in the All Children's Hospital NICU and the doctors say that he will most likely stay in the NICU until at least his scheduled due date of October 14th.
Wednesday (7/26), Chris and I went to see Kyle after my one week follow-up visit and were happy to find out that they had started him on breastmilk. He was only getting 1cc per every three hours but it was something.
Thursday (7/27), the doctors at All Children's put in a PICC line and removed the umbilical line. This was done for more long-term treatment. When my sister-in-law, Fran, took me to see Kyle, he was not at all happy about all the poking and prodding they had done. We're not able to hear his cries since he has tubes in him and his lungs are so tiny, but his expression howled volumes! The nurse had placed warm packs on his legs to warm them up. She said that it's common after having the PICC line put in and the umbilical line removed for infants to have leg spasms so the warm packs were to help with circulation in his legs.
The neonatologist, Dr. Stone, explained to me that Kyle had slight lung disease. She said it was common for preemies and just meant that he'd have to be on the ventillator longer than they had hoped. They were still going to continue trying to wean him slowly off the ventillator. I know that when she told me I must have looked panicked because that's how I felt but she assurred me that it was nothing as serious as with Eric and was just something they were keeping an eye on to be sure it didn't get more serious. Since Dr. Stone was the one that told me of the seriousness of Eric's condition, I trust her and know that she would inform me if there was anything immediately life-threatening.
Thursday evening, Dr. Stone called to tell me that one of Kyle's legs had not stopped spasming. An ultrasound of the blood vessels revealed that he had a blood clot in the leg. They called in a hemotologist (a blood specialist) who recommended a small dose of Heparin be administered. Dr. Stone explained that there was a possible risk that Heparin could cause bleeding on the brain so they were using the smallest dose possible, but without the Heparin Kyle could lose function of his leg. She assured me that they would be watching him very closely on the Heparin. I did not sleep well that night and was very relieved when the nurse practitioner called the next morning to inform us that the blood clot in Kyle's leg had broken up and they were now only concerned about tiny clots in a couple of his toes. They were continuing the Heparin to hopefully save the two tiny toes. I was relieved to know that he would not have to lose function of his entire leg, even if he does lose function of two toes.
The nurse practitioner also informed me that the Echocardiogram performed that morning had revealed that one valve of Kyle's heart that opens at birth was still open. She explained that the valve usually closes earlier than this but it was normal for preemies for it not to. She explained that another valve like this one had closed already which is really good. So, like with his lungs, this is nothing immediately life-threatening - just something they will keep an eye on for change.
When Chris and I went to see Kyle Friday night, his two littlest toes on his left foot were still very dark but I was happy to see that the rest of his leg had good color and he was looking pretty cosy and content. The nurse let me hold the small syringe of breastmilk to feed Kyle through a small tube. It was such a small thing but it felt good to take any part in his care. I'm looking forward to when he can be taken off the ventillator and I can hold him in my arms.
Wednesday (7/26), Chris and I went to see Kyle after my one week follow-up visit and were happy to find out that they had started him on breastmilk. He was only getting 1cc per every three hours but it was something.
Thursday (7/27), the doctors at All Children's put in a PICC line and removed the umbilical line. This was done for more long-term treatment. When my sister-in-law, Fran, took me to see Kyle, he was not at all happy about all the poking and prodding they had done. We're not able to hear his cries since he has tubes in him and his lungs are so tiny, but his expression howled volumes! The nurse had placed warm packs on his legs to warm them up. She said that it's common after having the PICC line put in and the umbilical line removed for infants to have leg spasms so the warm packs were to help with circulation in his legs.
The neonatologist, Dr. Stone, explained to me that Kyle had slight lung disease. She said it was common for preemies and just meant that he'd have to be on the ventillator longer than they had hoped. They were still going to continue trying to wean him slowly off the ventillator. I know that when she told me I must have looked panicked because that's how I felt but she assurred me that it was nothing as serious as with Eric and was just something they were keeping an eye on to be sure it didn't get more serious. Since Dr. Stone was the one that told me of the seriousness of Eric's condition, I trust her and know that she would inform me if there was anything immediately life-threatening.
Thursday evening, Dr. Stone called to tell me that one of Kyle's legs had not stopped spasming. An ultrasound of the blood vessels revealed that he had a blood clot in the leg. They called in a hemotologist (a blood specialist) who recommended a small dose of Heparin be administered. Dr. Stone explained that there was a possible risk that Heparin could cause bleeding on the brain so they were using the smallest dose possible, but without the Heparin Kyle could lose function of his leg. She assured me that they would be watching him very closely on the Heparin. I did not sleep well that night and was very relieved when the nurse practitioner called the next morning to inform us that the blood clot in Kyle's leg had broken up and they were now only concerned about tiny clots in a couple of his toes. They were continuing the Heparin to hopefully save the two tiny toes. I was relieved to know that he would not have to lose function of his entire leg, even if he does lose function of two toes.
The nurse practitioner also informed me that the Echocardiogram performed that morning had revealed that one valve of Kyle's heart that opens at birth was still open. She explained that the valve usually closes earlier than this but it was normal for preemies for it not to. She explained that another valve like this one had closed already which is really good. So, like with his lungs, this is nothing immediately life-threatening - just something they will keep an eye on for change.
When Chris and I went to see Kyle Friday night, his two littlest toes on his left foot were still very dark but I was happy to see that the rest of his leg had good color and he was looking pretty cosy and content. The nurse let me hold the small syringe of breastmilk to feed Kyle through a small tube. It was such a small thing but it felt good to take any part in his care. I'm looking forward to when he can be taken off the ventillator and I can hold him in my arms.
Milk and Money
After having no luck pumping milk since the C-section, I was thrilled when Monday and Tuesday, my milk finally came in. I had wanted to breastfeed both boys, despite many remarks from others that I would most likely give up breastfeeding pretty quickly with twin boys, so I had been disappointed that I wasn't able to get milk in for even one. It was even a source of pain for me that I wasn't able to provide that nutrient for them even though they weren't able to drink it yet. So when my milk finally came in, I felt a rush of joy. Since I breastfed Hannah, this was finally something that felt normal and right about having a newborn. I wasn't able to feel labor for my baby and I'm not yet able to hold my baby but at least I can give my baby the nutrients he needs. (FYI: For those that don't know it, suggesting that a mother-to-be will likely give up breastfeeding is not a source of comfort or support. If a mother CANNOT breastfeed or DOES give up breastfeeding on the other hand, telling her that "it's okay" IS a source of comfort and support.)
Tuesday night, while I was visiting Kyle with my parents and Chris was home in pain with the kidney stones, Chris received a call from his supervisor at work with some much-needed good news... He would be receiving bereavement pay for Monday, Tuesday and Wednesday. This news lightened the load some since we had thought that he would be getting no pay for these three days and I'm still out of work.
Tuesday night, while I was visiting Kyle with my parents and Chris was home in pain with the kidney stones, Chris received a call from his supervisor at work with some much-needed good news... He would be receiving bereavement pay for Monday, Tuesday and Wednesday. This news lightened the load some since we had thought that he would be getting no pay for these three days and I'm still out of work.
Sad Tasks
Monday (7/24) morning was a sad day since we had the task of making arrangements to lay to rest our dear little boy. Chris was still in pain from his kidney stones and I was still in pain from the C-section but the pain of Eric's death was still greater. Unfortunately, we did have to consider cost as we searched the web for information on burials, cremations and funerals. We decided to go with cremation by the Anderson-McQueen Funeral Home. We made arrangements to meet with them the next morning.
Tuesday (7/25), we met with a funeral director who discussed all the options with us. We could have a sort of viewing right before his cremation where they would place him in a bassinet or even hold him in a rocking chair but we turned down this offer since we had already said "goodbye" and our little Eric was no longer in the frail little body but was now in Heaven. We arranged for the release of the body from All Children's Hospital and filled out forms for the death certificate and obituary. No parent should ever have to make arrangements for their child to be laid to rest but the funeral director helped to make the task a little easier. He even arranged for the urn to be a tiny keepsake blue baby bootie.

Chris and I intend some day to have Eric's remains buried properly with a headstone but until we are ready for that, I believe the keepsake will be easier to look at than a plain, cold piece of pottery. I requested that Eric's footprints be taken for a necklace called a "Thumbie" to be made for me at a later time.
As we left the funeral home Tuesday afternoon, I felt as though my load had been lightened quite a bit. The arrangements were no longer looming over my head as a constant reminder of Eric's death. I felt more free to celebrate the life still with us, Kyle, and to celebrate that we had been able to have little Eric for at least the short amount of time we did.
Tuesday (7/25), we met with a funeral director who discussed all the options with us. We could have a sort of viewing right before his cremation where they would place him in a bassinet or even hold him in a rocking chair but we turned down this offer since we had already said "goodbye" and our little Eric was no longer in the frail little body but was now in Heaven. We arranged for the release of the body from All Children's Hospital and filled out forms for the death certificate and obituary. No parent should ever have to make arrangements for their child to be laid to rest but the funeral director helped to make the task a little easier. He even arranged for the urn to be a tiny keepsake blue baby bootie.

Chris and I intend some day to have Eric's remains buried properly with a headstone but until we are ready for that, I believe the keepsake will be easier to look at than a plain, cold piece of pottery. I requested that Eric's footprints be taken for a necklace called a "Thumbie" to be made for me at a later time.
As we left the funeral home Tuesday afternoon, I felt as though my load had been lightened quite a bit. The arrangements were no longer looming over my head as a constant reminder of Eric's death. I felt more free to celebrate the life still with us, Kyle, and to celebrate that we had been able to have little Eric for at least the short amount of time we did.
A Sweet Gesture
Sunday night, we went to see Kyle with my parents. When Chris left the NICU to trade with my father (only two visitors are allowed by the bedside at a time), the nurse came over to me and gave me a small gift. She handed me a small piece of clay with two sets of foot imprints - one next to beads that spelled out KYLE and the other next to beads that spelled out ERIC. The nurse said that another nurse had apparently done the imprints early the day before but she wasn't sure which one (we've found out since then it was a nurse named Valerie). Through my fresh tears, I asked the nurse to please thank the other nurse if she found out who it was. The small gift meant so much to me, especially after the sorrow of the night before.


Tuesday, July 25, 2006
Hello and Goodbye
July 19, 2006 we welcomed Frederic "Eric" Dean Foreman and Kyle Robert Foreman into the world, ahead of schedule.
July 22, 2006 Eric was welcomed into Heaven.
We celebrate our short time with Eric and Kyle's growing strength and appreciate all the thoughts and prayers.
.................................................
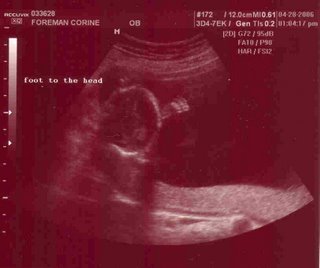
Wednesday, July 19th, I was feeling uncomfortable again already but as I waited with Carey for my appointment with Dr. Raimer, we were distracted with plans for the next day when she would be flying back to Indiana, and for my next few weeks before the twins' birth. But our thoughts were grounded very quickly when Dr. Raimer looked at the ultrasound and her face got very serious - something was wrong. She explained that they were going to transport me directly to Bayfront from the doctor's office and would likely deliver the babies by C-section either that same day or shortly thereafter. Dr. Montenegro was to meet me at Bayfront.
While the nurse wheeled me over to Bayfront in a wheelchair, Carey called Chris to inform him that he needed to leave work and meet us at Bayfront right away. I was brought to the assessment room at Bayfront where Dr. Montenegro looked at another ultrasound and confirmed that I would need to have a C-section immediately. I tried to remain calm while they prepped me for surgery but C-section was my greatest fear. They adminstered a spinal epidural and my feet and legs immediately started going numb. I felt tears well up as they strapped my arms out to the sides. I was afraid and no one could tell me if Chris had made it to the hospital in time. Just when I felt the panic build, a young doctor came to my side and told me that Chris had arrived and was getting gowned up for coming in. Carey had been put in a gown and mask just in case Chris didn't get there in time but at that moment I needed Chris.
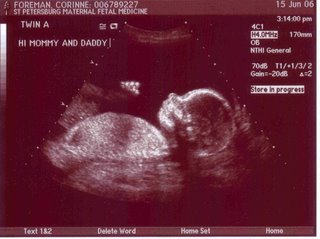
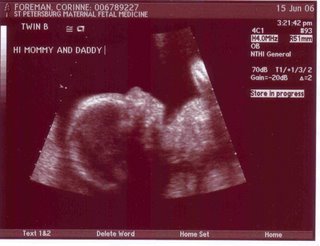
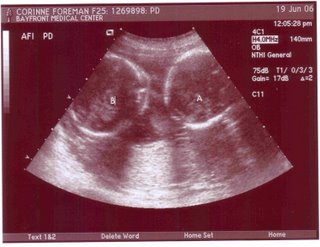
Chris stood by my side behind the barrier the whole time, comforting me and assuring me that everything was looking okay. When they began delivering the twins, Chris looked over the barrier and saw "Twin A" being delivered. I heard a whimper so tiny that I didn't think it was his cry until Chris told me it was. His lungs were so tiny that he could not give a full cry. As they delivered "Twin B", they found that the cord had been tangled around the two boys and actually tied in a knot. I didn't know until much later, but at the time of delivery, "Twin A" did not have any blood in his cord. Moments later and both boys would have been lost because of the tangled cord.
"Twin A" was 1 pound, 1 ounce born at 3:46pm. "Twin B" was 1 pound, 6 ounces born at 3:47pm. They were both rushed immediately to All Children's Hospital next door and Chris followed them there while the doctors gave me something to make me sleep. I don't remember anything after until late that night. They let me know when I woke up that both boys were stable, though they both had numerous problems and were very tiny. I was anxious to see them but I had to wait until the next day. While everyone was wanting me to decide on their names, I refused, insisting that I must see them first to be sure the names fit.
Thursday morning Carey and Chris wheeled me down to All Children's to see the boys but unfortunately we were only able to see "Twin A" since the doctors were doing rounds in the section of the Neonatal Intensive Care Unit (NICU) with "Twin B" so I could not decide still on the names. "Twin A" was a little frightening to see due to his small size. They had a blindfold covering half his face since he was under the bililight to treat his jaundice. They also him on a ventilator and IV and there were numerous tubes and wires on him. But he was my baby and beautiful to me. The nurse explained that their main concern right now was that he had not produced any urine yet and they could not determine if he had any kidney function but they said that it could just be temporary due to the twin-to-twin transfusion syndrome. They also had numerous concerns that were normal for any premature infant but I felt confident that he would fight the odds and be fine.
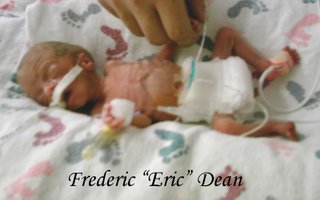
Later on, after Carey had said a reluctant goodbye and headed for the airport, Chris took me down again to see the twins with our friend, Jenn. This time I got to see both of them and felt certain of the names. "Twin A" was my little "Peaceful Leader", Frederic ("Eric") Dean, and "Twin B" was my "Handsome, Bright Fame", Kyle Robert.
The neonatologist took some time to talk to me and to Chris and explained that little Eric ("Twin A") had still not urinated and they were concerned since it had been about 24 hours but he could still turn around if he urinated in the next couple days. She also explained that Kyle ("Twin B") was having the opposite problem, where his bladder was filling more than it should and they were also concerned that his heart had a "thickened wall" caused by the excess blood from the twin-to-twin transfusion but with all their concerns, both boys were stable and looking beautiful.
Shortly after bringing me back to my room at Bayfront and saying goodbye to Jenn, Chris had to leave for home since his kidney stones were causing him a lot of pain. I felt pretty good with the nurses taking care of me and knowing that the twins weren't far away from me. My parents came by later on and brought me down a third time to see the boys. We took turns at the boys' bedsides since only two visitors are allowed by a bedside at a time. So my mom and I took pictures and cooed over one while my dad took pictures and cooed over the other.
I slept well Thursday night knowing my boys had names and were stable but Friday came with dark news and plenty of tears.
Friday afternoon, Chris was unable to make it out to the hospital. He was in pain from the kidney stones and was on medication that didn't allow him to drive. So his mother came to keep me company and to bring me down for a visit to the NICU. I was in a happy mood on the way down there. Though there were concerns, I felt certain that my boys were fighters. But when the neonatologist came to speak to me, the news was not good. Eric had still not urinated and it was not looking like he had functioning kidneys. The fluid in him was building up around his other organs and if he couldn't urinate, the fluid would eventually be toxic in his body. I tried to be optomistic but the doctor informed me that if his kidneys did not begin to function on their own, there was nothing that could be done. He was too small for a transplant or dialysis and the only option would be to wait for his body to give up.
Chris' mom, Marcy, brought me back to my room sobbing. I was no longer optomistic. I was no longer certain that he could fight the odds. If his kidneys were not functioning, he wasn't equipped to fight. Marcy left so that she could pick up Chris' sister, Rachel, from the airport later that night. Rachel has been in the Army in New York and is scheduled for deployment to Iraq soon, but she got special leave in order to come and be with us.
I called Chris but he was still unable to make it to the hospital because of the kidney stones and pain medication. I called my parents and asked them to come over to be with me. My sobbing was uncontrollable until I called my sister. She comforted me and reminded me that there was still a chance that Eric might urinate and turn things around. She also reminded me that I very nearly didn't have Eric at all - or even Kyle, for that matter - and they had proven to be fighters already.
 My parents came later and brought me down again to see the boys. This time, I spent almost the whole time by Eric's side and I made sure to touch him as much as I could. I wanted to be sure to have memories to hold onto. The nurse took him off the bililight and took his blindfold off for a little while so we could see his face better. Eric gripped his tiny little knuckles around my finger and blew tiny spit bubbles. He even curled his lip into a slight smile for me. The nurse explained that he still hadn't urinated and his color was starting to look dusky, which was a sign that the fluid was building around his other organs.
My parents came later and brought me down again to see the boys. This time, I spent almost the whole time by Eric's side and I made sure to touch him as much as I could. I wanted to be sure to have memories to hold onto. The nurse took him off the bililight and took his blindfold off for a little while so we could see his face better. Eric gripped his tiny little knuckles around my finger and blew tiny spit bubbles. He even curled his lip into a slight smile for me. The nurse explained that he still hadn't urinated and his color was starting to look dusky, which was a sign that the fluid was building around his other organs.
Friday night was hard for me. The uncontrollable sobbing came often. The night nurse, Angela, came in to check on me and asked about the boys. When I told her, I started crying again and she scooped me up into her arms and began crying and praying with me. It was very comforting.
In the middle of the night, All Children's called and for a moment, I got my hopes up. I had told them to call me if Eric urinated, no matter what the time. But when the nurse spoke, I knew that it wasn't good news. In fact, it was very nearly very bad news. Eric's heart rate had gone down to critical and they had manually stabilized him using a bag. They had called in the "code team" but he had stabilized and they were able to put him back on the ventilator. It was comforting to know that I was close enough to get there in a matter of minutes if he had not stabilized. I dreaded the next day because they were planning on discharging me.
Saturday morning, Chris packed Hannah up to go to my cousin's house in Lake Wales for the week. My parents drove her out there. Chris' mom picked him up shortly afterward to take him to Bayfront. Meanwhile, the doctor told me they were discharging me but the nurses had said I could stay until 10 pm if I needed to. I called Ronald McDonald House to arrange that I could stay there that night in order to be close to the boys at All Children's. They said I needed to be there by 9 pm to check in and I needed to have someone stay with me or I needed to have the post C-section staples removed. The doctor said they could go ahead and remove the staples without any problem.
Chris arrived with his mother and his sister, Rachel, around lunchtime so we ate our lunch quickly before heading down to the NICU. My heart sank as soon as I saw Eric. It was clear that the night had not been good to him. His tiny body was swollen with fluid and his color had turned such a dark grey, he was almost black. I asked to see the neonatologist. He confirmed that Eric was not showing any sign of improvement and would only be with us for a very short time. They had started him on pain medication. Chris and I cried over our precious little one. Our hearts were both breaking.
Though our other small boy was looking a lot better and the nurses told us he had even peed his bed when they had changed him earlier, we were not comforted. The neonatologist informed us that we would need to decide whether we wanted to have the hospital perform code on Eric if he started to fade or if we wanted to take him off the medications and tubes that were keeping him alive and say goodbye to him. Chris and I agreed that we didn't want to prolong our little boy's pain but I insisted we wait for my parents to be there. We called my mom and dad and asked them to rush back from Lake Wales.
I decided that I wanted to return to Bayfront long enough for them to discharge me and cancel my reservation at Ronald McDonald House so I could stay as late as necessary in the NICU. I was determined not to leave Eric alone, afraid that he might die with no one there. Marcy promised to stay by Eric's side and make sure he was not alone while I settled things at Bayfront.
My discharge took longer than I would've liked because the nurse that was on duty was not aware of my situation and did not understand the urgency. I had to explain the situation which took away all of my strength in order for her to understand that I needed the staples removed, even though I was not staying at the Ronald McDonald House (RMH) that night because I may need to stay at the RMH the next night. She had wanted a definite answer as to whether or not I'd be staying at the RMH and I tearfully explained that I didn't know if my infant would be alive the following day so I couldn't be sure. She finally removed the staples and gave me my discharge papers and we returned to the NICU. By that time, my parents, Chris' dad, and Jenn had all arrived.
Once we returned to the NICU, I felt an odd peace. In a few moments, I would be able to hold my precious little one and give him the best thing I could - an end to the pain while surrounded by love.
We had to wait for the chaplain and the neonatologist and I sat with Kyle for a moment while we waited. Kyle looked so strong and healthy compared to his brother and his nurse assurred me that he was indeed stronger and steadily getting better. It was comforting but after a moment, I had to return to Eric's bedside and face the hardest event of my life.
 The NICU waived the rules and we all stood
The NICU waived the rules and we all stood  (me, Chris, my parents, his parents, Rachel and Jenn) by Eric's bedside. They allowed me to hold his tiny body cradled in my arms while the life support was still on him and when they removed the life support, we all brought him into the chaplain's office to say goodbye. We all said goodbye and held him during the few minutes and then Eric's face spread into a giant smile as he breathed his last breath.
(me, Chris, my parents, his parents, Rachel and Jenn) by Eric's bedside. They allowed me to hold his tiny body cradled in my arms while the life support was still on him and when they removed the life support, we all brought him into the chaplain's office to say goodbye. We all said goodbye and held him during the few minutes and then Eric's face spread into a giant smile as he breathed his last breath.
The neonatologist pronounced time of death and while I sat there crying, the other women cleaned Eric up with the help of the nurse. They provided a small box for keepsakes like Eric's hospital bracelet and blood pressure cuff and such. One of the nurses had even made a small bracelet from ribbon and beads that said "ERIC". The chaplain spoke a few words of comfort and we all left the hospital feeling drained and exhausted.
I know from his smile in the end that he had met the welcoming committee - all the loved ones who have passed before and I know that he was no longer in pain. He no longer needs kidneys where he is now and I know that my grandfather and Chris' grandfather, as well as my Aunt Sandie and many others, are all holding him now and he's in good hands. Chris and I miss him dearly and will always hold a special place for him in our hearts.

July 22, 2006 Eric was welcomed into Heaven.
We celebrate our short time with Eric and Kyle's growing strength and appreciate all the thoughts and prayers.
.................................................
Wednesday, July 19th, I was feeling uncomfortable again already but as I waited with Carey for my appointment with Dr. Raimer, we were distracted with plans for the next day when she would be flying back to Indiana, and for my next few weeks before the twins' birth. But our thoughts were grounded very quickly when Dr. Raimer looked at the ultrasound and her face got very serious - something was wrong. She explained that they were going to transport me directly to Bayfront from the doctor's office and would likely deliver the babies by C-section either that same day or shortly thereafter. Dr. Montenegro was to meet me at Bayfront.
While the nurse wheeled me over to Bayfront in a wheelchair, Carey called Chris to inform him that he needed to leave work and meet us at Bayfront right away. I was brought to the assessment room at Bayfront where Dr. Montenegro looked at another ultrasound and confirmed that I would need to have a C-section immediately. I tried to remain calm while they prepped me for surgery but C-section was my greatest fear. They adminstered a spinal epidural and my feet and legs immediately started going numb. I felt tears well up as they strapped my arms out to the sides. I was afraid and no one could tell me if Chris had made it to the hospital in time. Just when I felt the panic build, a young doctor came to my side and told me that Chris had arrived and was getting gowned up for coming in. Carey had been put in a gown and mask just in case Chris didn't get there in time but at that moment I needed Chris.
Chris stood by my side behind the barrier the whole time, comforting me and assuring me that everything was looking okay. When they began delivering the twins, Chris looked over the barrier and saw "Twin A" being delivered. I heard a whimper so tiny that I didn't think it was his cry until Chris told me it was. His lungs were so tiny that he could not give a full cry. As they delivered "Twin B", they found that the cord had been tangled around the two boys and actually tied in a knot. I didn't know until much later, but at the time of delivery, "Twin A" did not have any blood in his cord. Moments later and both boys would have been lost because of the tangled cord.
"Twin A" was 1 pound, 1 ounce born at 3:46pm. "Twin B" was 1 pound, 6 ounces born at 3:47pm. They were both rushed immediately to All Children's Hospital next door and Chris followed them there while the doctors gave me something to make me sleep. I don't remember anything after until late that night. They let me know when I woke up that both boys were stable, though they both had numerous problems and were very tiny. I was anxious to see them but I had to wait until the next day. While everyone was wanting me to decide on their names, I refused, insisting that I must see them first to be sure the names fit.
Thursday morning Carey and Chris wheeled me down to All Children's to see the boys but unfortunately we were only able to see "Twin A" since the doctors were doing rounds in the section of the Neonatal Intensive Care Unit (NICU) with "Twin B" so I could not decide still on the names. "Twin A" was a little frightening to see due to his small size. They had a blindfold covering half his face since he was under the bililight to treat his jaundice. They also him on a ventilator and IV and there were numerous tubes and wires on him. But he was my baby and beautiful to me. The nurse explained that their main concern right now was that he had not produced any urine yet and they could not determine if he had any kidney function but they said that it could just be temporary due to the twin-to-twin transfusion syndrome. They also had numerous concerns that were normal for any premature infant but I felt confident that he would fight the odds and be fine.
Later on, after Carey had said a reluctant goodbye and headed for the airport, Chris took me down again to see the twins with our friend, Jenn. This time I got to see both of them and felt certain of the names. "Twin A" was my little "Peaceful Leader", Frederic ("Eric") Dean, and "Twin B" was my "Handsome, Bright Fame", Kyle Robert.
The neonatologist took some time to talk to me and to Chris and explained that little Eric ("Twin A") had still not urinated and they were concerned since it had been about 24 hours but he could still turn around if he urinated in the next couple days. She also explained that Kyle ("Twin B") was having the opposite problem, where his bladder was filling more than it should and they were also concerned that his heart had a "thickened wall" caused by the excess blood from the twin-to-twin transfusion but with all their concerns, both boys were stable and looking beautiful.
Shortly after bringing me back to my room at Bayfront and saying goodbye to Jenn, Chris had to leave for home since his kidney stones were causing him a lot of pain. I felt pretty good with the nurses taking care of me and knowing that the twins weren't far away from me. My parents came by later on and brought me down a third time to see the boys. We took turns at the boys' bedsides since only two visitors are allowed by a bedside at a time. So my mom and I took pictures and cooed over one while my dad took pictures and cooed over the other.
I slept well Thursday night knowing my boys had names and were stable but Friday came with dark news and plenty of tears.
Friday afternoon, Chris was unable to make it out to the hospital. He was in pain from the kidney stones and was on medication that didn't allow him to drive. So his mother came to keep me company and to bring me down for a visit to the NICU. I was in a happy mood on the way down there. Though there were concerns, I felt certain that my boys were fighters. But when the neonatologist came to speak to me, the news was not good. Eric had still not urinated and it was not looking like he had functioning kidneys. The fluid in him was building up around his other organs and if he couldn't urinate, the fluid would eventually be toxic in his body. I tried to be optomistic but the doctor informed me that if his kidneys did not begin to function on their own, there was nothing that could be done. He was too small for a transplant or dialysis and the only option would be to wait for his body to give up.
Chris' mom, Marcy, brought me back to my room sobbing. I was no longer optomistic. I was no longer certain that he could fight the odds. If his kidneys were not functioning, he wasn't equipped to fight. Marcy left so that she could pick up Chris' sister, Rachel, from the airport later that night. Rachel has been in the Army in New York and is scheduled for deployment to Iraq soon, but she got special leave in order to come and be with us.
I called Chris but he was still unable to make it to the hospital because of the kidney stones and pain medication. I called my parents and asked them to come over to be with me. My sobbing was uncontrollable until I called my sister. She comforted me and reminded me that there was still a chance that Eric might urinate and turn things around. She also reminded me that I very nearly didn't have Eric at all - or even Kyle, for that matter - and they had proven to be fighters already.
 My parents came later and brought me down again to see the boys. This time, I spent almost the whole time by Eric's side and I made sure to touch him as much as I could. I wanted to be sure to have memories to hold onto. The nurse took him off the bililight and took his blindfold off for a little while so we could see his face better. Eric gripped his tiny little knuckles around my finger and blew tiny spit bubbles. He even curled his lip into a slight smile for me. The nurse explained that he still hadn't urinated and his color was starting to look dusky, which was a sign that the fluid was building around his other organs.
My parents came later and brought me down again to see the boys. This time, I spent almost the whole time by Eric's side and I made sure to touch him as much as I could. I wanted to be sure to have memories to hold onto. The nurse took him off the bililight and took his blindfold off for a little while so we could see his face better. Eric gripped his tiny little knuckles around my finger and blew tiny spit bubbles. He even curled his lip into a slight smile for me. The nurse explained that he still hadn't urinated and his color was starting to look dusky, which was a sign that the fluid was building around his other organs.Friday night was hard for me. The uncontrollable sobbing came often. The night nurse, Angela, came in to check on me and asked about the boys. When I told her, I started crying again and she scooped me up into her arms and began crying and praying with me. It was very comforting.
In the middle of the night, All Children's called and for a moment, I got my hopes up. I had told them to call me if Eric urinated, no matter what the time. But when the nurse spoke, I knew that it wasn't good news. In fact, it was very nearly very bad news. Eric's heart rate had gone down to critical and they had manually stabilized him using a bag. They had called in the "code team" but he had stabilized and they were able to put him back on the ventilator. It was comforting to know that I was close enough to get there in a matter of minutes if he had not stabilized. I dreaded the next day because they were planning on discharging me.
Saturday morning, Chris packed Hannah up to go to my cousin's house in Lake Wales for the week. My parents drove her out there. Chris' mom picked him up shortly afterward to take him to Bayfront. Meanwhile, the doctor told me they were discharging me but the nurses had said I could stay until 10 pm if I needed to. I called Ronald McDonald House to arrange that I could stay there that night in order to be close to the boys at All Children's. They said I needed to be there by 9 pm to check in and I needed to have someone stay with me or I needed to have the post C-section staples removed. The doctor said they could go ahead and remove the staples without any problem.
Chris arrived with his mother and his sister, Rachel, around lunchtime so we ate our lunch quickly before heading down to the NICU. My heart sank as soon as I saw Eric. It was clear that the night had not been good to him. His tiny body was swollen with fluid and his color had turned such a dark grey, he was almost black. I asked to see the neonatologist. He confirmed that Eric was not showing any sign of improvement and would only be with us for a very short time. They had started him on pain medication. Chris and I cried over our precious little one. Our hearts were both breaking.
Though our other small boy was looking a lot better and the nurses told us he had even peed his bed when they had changed him earlier, we were not comforted. The neonatologist informed us that we would need to decide whether we wanted to have the hospital perform code on Eric if he started to fade or if we wanted to take him off the medications and tubes that were keeping him alive and say goodbye to him. Chris and I agreed that we didn't want to prolong our little boy's pain but I insisted we wait for my parents to be there. We called my mom and dad and asked them to rush back from Lake Wales.
I decided that I wanted to return to Bayfront long enough for them to discharge me and cancel my reservation at Ronald McDonald House so I could stay as late as necessary in the NICU. I was determined not to leave Eric alone, afraid that he might die with no one there. Marcy promised to stay by Eric's side and make sure he was not alone while I settled things at Bayfront.
My discharge took longer than I would've liked because the nurse that was on duty was not aware of my situation and did not understand the urgency. I had to explain the situation which took away all of my strength in order for her to understand that I needed the staples removed, even though I was not staying at the Ronald McDonald House (RMH) that night because I may need to stay at the RMH the next night. She had wanted a definite answer as to whether or not I'd be staying at the RMH and I tearfully explained that I didn't know if my infant would be alive the following day so I couldn't be sure. She finally removed the staples and gave me my discharge papers and we returned to the NICU. By that time, my parents, Chris' dad, and Jenn had all arrived.
Once we returned to the NICU, I felt an odd peace. In a few moments, I would be able to hold my precious little one and give him the best thing I could - an end to the pain while surrounded by love.
We had to wait for the chaplain and the neonatologist and I sat with Kyle for a moment while we waited. Kyle looked so strong and healthy compared to his brother and his nurse assurred me that he was indeed stronger and steadily getting better. It was comforting but after a moment, I had to return to Eric's bedside and face the hardest event of my life.
 The NICU waived the rules and we all stood
The NICU waived the rules and we all stood  (me, Chris, my parents, his parents, Rachel and Jenn) by Eric's bedside. They allowed me to hold his tiny body cradled in my arms while the life support was still on him and when they removed the life support, we all brought him into the chaplain's office to say goodbye. We all said goodbye and held him during the few minutes and then Eric's face spread into a giant smile as he breathed his last breath.
(me, Chris, my parents, his parents, Rachel and Jenn) by Eric's bedside. They allowed me to hold his tiny body cradled in my arms while the life support was still on him and when they removed the life support, we all brought him into the chaplain's office to say goodbye. We all said goodbye and held him during the few minutes and then Eric's face spread into a giant smile as he breathed his last breath.The neonatologist pronounced time of death and while I sat there crying, the other women cleaned Eric up with the help of the nurse. They provided a small box for keepsakes like Eric's hospital bracelet and blood pressure cuff and such. One of the nurses had even made a small bracelet from ribbon and beads that said "ERIC". The chaplain spoke a few words of comfort and we all left the hospital feeling drained and exhausted.
I know from his smile in the end that he had met the welcoming committee - all the loved ones who have passed before and I know that he was no longer in pain. He no longer needs kidneys where he is now and I know that my grandfather and Chris' grandfather, as well as my Aunt Sandie and many others, are all holding him now and he's in good hands. Chris and I miss him dearly and will always hold a special place for him in our hearts.

Monday, July 17, 2006
5th Amnio Reduction
July 17th another amnio reduction was performed removing 4 liters of fluid. I called ahead to make sure that Dr. Raimer would be the doctor on call and they put me up in a labor and delivery room again. Dr. Raimer had them administer Demerol before they began the reduction to ensure the least discomfort. The Demerol also kept my uterus relaxed and made the reduction quick and painless. I didn't even have any contractions after the reduction and they discharged me the same day.
Tuesday, July 11, 2006
4th Amnio Reduction
Sure enough, after a night with no sleep, Monday morning I went in to the hospital again for yet another amnio reduction. This time, however, was a lot more pleasant than last time. First of all, Dr. Raimer was on call instead of Dr. Prieto. She had performed the first amnio reduction, which had been virtually painless so I felt good about her doing this one. As I walked up to the antepartum nurses station, I right away saw Dr. Raimer. Luckily, she wore a nice white lab coat with her name embroidered on the front because I didn't recognize her (I was pretty out of it during the first amnio reduction). They checked me right in to a birthing suite instead of one of the broom closet antepartum rooms and the nurses were all helpful and attentive.
They didn't give me any problem about drinking juice and water or taking my regular prescriptions before the procedures and even brought me some crackers in case I got hungry beforehand. Last time, I had to wait 9 hours before they gave me approval to eat, drink or take my prescriptions!
Once I got settled into the birthing suite, I noticed the prep table had only one 1 liter bottle for fluid so when the nurse came in I mentioned that she might want to get more since I had been averaging 5 liters per a reduction. She went and got a few more of the larger 2 liter bottles.
When Dr. Raimer came in and started the procedure, I was a little nervous because the last one had been so incredibly painful but once she started I was pleased to find that it started as comfortable as the first one. A little ways into it (almost 2 liters into it), though, and it started hurting again so I let her know. She pointed out on the ultrasound screen a bulge around where the needle was inserted and explained that my uterus was contracting around the needle. She also ordered the nurse to get me a shot of Morphine for the pain and had the resident assisting her adjust the needle to a more comfortable angle. Before the morphine was even in my system, the pain almost completely went away from just adjusting the needle. I was so glad to see that Dr. Raimer was attentive to my discomfort and quick to relieve it.
As with the last couple of reductions, the membrane kept brushing past the needle and snagging because of the vacuum. But, rather than just wiggle the needle up and down to un-snag it as Dr. Prieto had done (very uncomfortable), Dr. Raimer removed the vacuum just long enough to inject a few air bubbles through the needle using an empty sterile syringe, pushing the membrane away. It was kind of funny to see the little air bubbles on the ultrasound screen and watch them get sucked back up into the vacuum (babies' first bubble bath).
Dr. Raimer and the assisting resident continued to have light conversation with me rather than around me during the entire procedure, informing me the whole time of how the procedure was going. Dr. Raimer even mentioned that they only had to use one tap because according to my chart, they suspected that during one of the first amnio reductions, a small hole may have been made in the membranes dividing the twins' sacks. This would explain why the fluid has been even on both twins since after the first amnio reduction. She seemed to think that I had already been informed of this detail, which I had not. I was quite surprised at how quickly the procedure was over with, especially when I saw that the third 2 liter bottle was actually FULL. They removed 6 liters this time!
Almost as soon as the needle was out and they were cleaning me up after the amnio reduction, I started feeling the effects of the Morphine combined with nearly 24 hours without sleep. I felt the relief of having the 6 liters removed. I could breathe easier than I had in days without the pressure of so much fluid. I was perfectly comfortable and happy as they put in my IV and gave me a shot of Betamethasone (a steroid to help the twins' lungs develop in case they need to be delivered before term).
I mentioned to the nurse that I liked Dr. Raimer a lot more than Dr. Prieto and how impressed I was by her. The nurse looked as though she agreed with my opinion of Dr. Prieto but only said, "She should know what she's doing. She's got children of her own so she's been there." My sister asked how many children Dr. Raimer had and the nurse said "6 or 7, including a set of twins".
As soon as I'd slept for a little while, the contractions had stopped, and the Morphine had worn off, they gave me a tray of food before discharging me around 8:30pm. It was nice not to have to stay overnight for a change. I had worried that they would keep me overnight because the contraction monitor was picking up the twins' movements as they pushed themselves against where the monitor was and it made it look like I was still contracting. But they let me go with instructions to take the Procardia every four hours instead of six and to go to the Dr.'s office this afternoon (Tuesday) for a second injection of the Betamethasone.
Last night I had no problem falling asleep and staying asleep all night, only waking up long enough to take my prescriptions during the night.
They didn't give me any problem about drinking juice and water or taking my regular prescriptions before the procedures and even brought me some crackers in case I got hungry beforehand. Last time, I had to wait 9 hours before they gave me approval to eat, drink or take my prescriptions!
Once I got settled into the birthing suite, I noticed the prep table had only one 1 liter bottle for fluid so when the nurse came in I mentioned that she might want to get more since I had been averaging 5 liters per a reduction. She went and got a few more of the larger 2 liter bottles.
When Dr. Raimer came in and started the procedure, I was a little nervous because the last one had been so incredibly painful but once she started I was pleased to find that it started as comfortable as the first one. A little ways into it (almost 2 liters into it), though, and it started hurting again so I let her know. She pointed out on the ultrasound screen a bulge around where the needle was inserted and explained that my uterus was contracting around the needle. She also ordered the nurse to get me a shot of Morphine for the pain and had the resident assisting her adjust the needle to a more comfortable angle. Before the morphine was even in my system, the pain almost completely went away from just adjusting the needle. I was so glad to see that Dr. Raimer was attentive to my discomfort and quick to relieve it.
As with the last couple of reductions, the membrane kept brushing past the needle and snagging because of the vacuum. But, rather than just wiggle the needle up and down to un-snag it as Dr. Prieto had done (very uncomfortable), Dr. Raimer removed the vacuum just long enough to inject a few air bubbles through the needle using an empty sterile syringe, pushing the membrane away. It was kind of funny to see the little air bubbles on the ultrasound screen and watch them get sucked back up into the vacuum (babies' first bubble bath).
Dr. Raimer and the assisting resident continued to have light conversation with me rather than around me during the entire procedure, informing me the whole time of how the procedure was going. Dr. Raimer even mentioned that they only had to use one tap because according to my chart, they suspected that during one of the first amnio reductions, a small hole may have been made in the membranes dividing the twins' sacks. This would explain why the fluid has been even on both twins since after the first amnio reduction. She seemed to think that I had already been informed of this detail, which I had not. I was quite surprised at how quickly the procedure was over with, especially when I saw that the third 2 liter bottle was actually FULL. They removed 6 liters this time!
Almost as soon as the needle was out and they were cleaning me up after the amnio reduction, I started feeling the effects of the Morphine combined with nearly 24 hours without sleep. I felt the relief of having the 6 liters removed. I could breathe easier than I had in days without the pressure of so much fluid. I was perfectly comfortable and happy as they put in my IV and gave me a shot of Betamethasone (a steroid to help the twins' lungs develop in case they need to be delivered before term).
I mentioned to the nurse that I liked Dr. Raimer a lot more than Dr. Prieto and how impressed I was by her. The nurse looked as though she agreed with my opinion of Dr. Prieto but only said, "She should know what she's doing. She's got children of her own so she's been there." My sister asked how many children Dr. Raimer had and the nurse said "6 or 7, including a set of twins".
As soon as I'd slept for a little while, the contractions had stopped, and the Morphine had worn off, they gave me a tray of food before discharging me around 8:30pm. It was nice not to have to stay overnight for a change. I had worried that they would keep me overnight because the contraction monitor was picking up the twins' movements as they pushed themselves against where the monitor was and it made it look like I was still contracting. But they let me go with instructions to take the Procardia every four hours instead of six and to go to the Dr.'s office this afternoon (Tuesday) for a second injection of the Betamethasone.
Last night I had no problem falling asleep and staying asleep all night, only waking up long enough to take my prescriptions during the night.
Monday, July 10, 2006
The Other Foreman
All my posts have been about me and Hannah and the twins so here's an update on the other Foreman, Chris:
Chris has been battling kidney stones yet again. He had an appointment with the new doctor last Monday and was scheduled for an IVP Friday morning. An IVP is basically an X-ray where they inject dye into the system beforehand to show more detail. According to the IVP results, he's got a kidney stone partially blocking on one side so he needs to schedule an appointment with a urologist as soon as possible. We're going with a different urologist this time around. Dr. Krauss at Bayfront has treated him previously but doesn't seem to be big on the prevention of kidney stones - just the treatment. Chris has had kidney stones about every 4-6 months on average since we got married and all we know is that they are caused by a hormonal imbalance that makes it so his body doesn't break down calcium like it should, so instead it builds up and creates stones in his kidneys.
I'll try to update the blog as we find out more.
Chris has been battling kidney stones yet again. He had an appointment with the new doctor last Monday and was scheduled for an IVP Friday morning. An IVP is basically an X-ray where they inject dye into the system beforehand to show more detail. According to the IVP results, he's got a kidney stone partially blocking on one side so he needs to schedule an appointment with a urologist as soon as possible. We're going with a different urologist this time around. Dr. Krauss at Bayfront has treated him previously but doesn't seem to be big on the prevention of kidney stones - just the treatment. Chris has had kidney stones about every 4-6 months on average since we got married and all we know is that they are caused by a hormonal imbalance that makes it so his body doesn't break down calcium like it should, so instead it builds up and creates stones in his kidneys.
I'll try to update the blog as we find out more.
26 Weeks
Well, last Wednesday I had another appointment at Dr. Prieto's office. This one was actually officially my "transfer of care" appointment so I thought more questions would be answered and I'd get a little more time actually talking to the doctor (or at least the nurse practitioner) about my current conditions. However, other than taking my vitals and asking the same family medical history questions that the hospital asks, the appointment was just like the other appointments. When I tried asking the nurse practitioner questions about my bed rest and Cholestasis and such, she just said "Ask Dr. Prieto when you see him".
So after yet another ultrasound (during which, Dr. Prieto mumbled to the ultrasound tech as usual and barely glanced in my direction), the doctor said that we would go ahead and plan for another amnio reduction next Thursday after another ultrasound appointment and began to leave the room. This time I stopped him and said, "I have a few questions, actually."
I told him that I had researched Cholestasis on the web and found information leading me to believe that it is rather serious and I was especially concerned that one of the side effects of Cholestasis is a vitamin K deficiency that can cause the mother to bleed out after giving birth. I mentioned that this may be of great concern since a couple days before I had bit lip and it had continued to bleed for a half hour! I asked if there was any way I could take a vitamin K supplement and his response was a slight roll of the eye and, basically, that he didn't see any reason for it but if I really wanted to try it, I should just get it over-the-counter. (I learned later on that you cannot get vitamin K supplements over-the-counter. They are prescription only.)
Then I told him that I would like to know what type of bed rest I'm on since a nurse at Bayfront said that there are several types such as complete bed rest, modified bed rest and pelvic bed rest. The doctor actually chuckled at this but the nurse in the room timidly said that there were indeed different types of bed rest so the doctor clarified that I'm "on bed rest but not bed ridden". (So clear!) When I tried to get a little clearer explaination, he basically said that I'm on bed rest to prevent preterm labor but I'm most likely going to have preterm labor anyway. (Again, so clear.)
As I was leaving the doctor's office I stopped to talk to the receptionist. I had received the Medicaid cards for myself, Hannah and "Baby A of Foreman" and Baby B of Foreman" so I asked how that worked since I had Aetna as my primary insurance. Turns out, this doctor's office doesn't accept Medicaid.
Friday morning I received a certified mail from my work saying that I was terminated effective July 7th and my benefits would continue to the end of July. They had warned me of this a few weeks ago but I was hoping that something would change like I could return to work. I know many of you are thinking, "They can't fire you for not working if it's a medical reason". However, Family Medical Leave Act (FMLA) only protects you if you have worked for the employer for a full 12 months. I started January 30th of this year. So after all this baby drama is over and the twins are healthy and outside my belly, I'll be looking for a new job. I may be able to get a job for the same company but by then they'll definitely have filled my current position and I really liked the department I was in.
On Friday afternoon, my sister brought me and Hannah to the WIC office to sign up for assistance. I wasn't feeling my best after sitting up for over an hour and a half but when we left, I had WIC vouchers for three months. Hannah and I each had to have our fingers pricked to check our iron levels. Hannah took it like a champ, not even crying for a second and her iron levels were perfect. Mine however were slightly anemic and I was told I need to increase the iron in my diet.
Now it's the middle of Sunday night/Monday morning pretty much and I'm just waiting for time to go by. As soon as the hospital registration office opens, I plan to call them and ask how to go about switching doctors considering my insurance coverage ends the end of this month and Dr. Prieto doesn't take Medicaid... and I don't really like Dr. Prieto anyway. My only concern is that I don't know how many other doctors can perform amnio reductions since that was apparently the reason Dr. Igel had needed to transfer my care in the first place.
I'm pretty sure I'm going to need another amnio reduction today. The entire day I've been uncomfortable and short of breath from the excess fluid. I just hope I can work it so that Dr. Prieto isn't the one to do it this time.
I'm having a hard time not getting discouraged with all that's happening. My sister leaves again for Indiana on July 20th and I'm not sure what I'm going to do with her gone. We've had to take Hannah out of daycare during all this because it costs too much and I'm not sure how I'm going to care for her alone during the days. My mom had been helping before Carey came down but my mom starts a new job today (Monday). At least her new job is really close to here so she can actually come by on her lunch breaks, which should help some.
So after yet another ultrasound (during which, Dr. Prieto mumbled to the ultrasound tech as usual and barely glanced in my direction), the doctor said that we would go ahead and plan for another amnio reduction next Thursday after another ultrasound appointment and began to leave the room. This time I stopped him and said, "I have a few questions, actually."
I told him that I had researched Cholestasis on the web and found information leading me to believe that it is rather serious and I was especially concerned that one of the side effects of Cholestasis is a vitamin K deficiency that can cause the mother to bleed out after giving birth. I mentioned that this may be of great concern since a couple days before I had bit lip and it had continued to bleed for a half hour! I asked if there was any way I could take a vitamin K supplement and his response was a slight roll of the eye and, basically, that he didn't see any reason for it but if I really wanted to try it, I should just get it over-the-counter. (I learned later on that you cannot get vitamin K supplements over-the-counter. They are prescription only.)
Then I told him that I would like to know what type of bed rest I'm on since a nurse at Bayfront said that there are several types such as complete bed rest, modified bed rest and pelvic bed rest. The doctor actually chuckled at this but the nurse in the room timidly said that there were indeed different types of bed rest so the doctor clarified that I'm "on bed rest but not bed ridden". (So clear!) When I tried to get a little clearer explaination, he basically said that I'm on bed rest to prevent preterm labor but I'm most likely going to have preterm labor anyway. (Again, so clear.)
As I was leaving the doctor's office I stopped to talk to the receptionist. I had received the Medicaid cards for myself, Hannah and "Baby A of Foreman" and Baby B of Foreman" so I asked how that worked since I had Aetna as my primary insurance. Turns out, this doctor's office doesn't accept Medicaid.
Friday morning I received a certified mail from my work saying that I was terminated effective July 7th and my benefits would continue to the end of July. They had warned me of this a few weeks ago but I was hoping that something would change like I could return to work. I know many of you are thinking, "They can't fire you for not working if it's a medical reason". However, Family Medical Leave Act (FMLA) only protects you if you have worked for the employer for a full 12 months. I started January 30th of this year. So after all this baby drama is over and the twins are healthy and outside my belly, I'll be looking for a new job. I may be able to get a job for the same company but by then they'll definitely have filled my current position and I really liked the department I was in.
On Friday afternoon, my sister brought me and Hannah to the WIC office to sign up for assistance. I wasn't feeling my best after sitting up for over an hour and a half but when we left, I had WIC vouchers for three months. Hannah and I each had to have our fingers pricked to check our iron levels. Hannah took it like a champ, not even crying for a second and her iron levels were perfect. Mine however were slightly anemic and I was told I need to increase the iron in my diet.
Now it's the middle of Sunday night/Monday morning pretty much and I'm just waiting for time to go by. As soon as the hospital registration office opens, I plan to call them and ask how to go about switching doctors considering my insurance coverage ends the end of this month and Dr. Prieto doesn't take Medicaid... and I don't really like Dr. Prieto anyway. My only concern is that I don't know how many other doctors can perform amnio reductions since that was apparently the reason Dr. Igel had needed to transfer my care in the first place.
I'm pretty sure I'm going to need another amnio reduction today. The entire day I've been uncomfortable and short of breath from the excess fluid. I just hope I can work it so that Dr. Prieto isn't the one to do it this time.
I'm having a hard time not getting discouraged with all that's happening. My sister leaves again for Indiana on July 20th and I'm not sure what I'm going to do with her gone. We've had to take Hannah out of daycare during all this because it costs too much and I'm not sure how I'm going to care for her alone during the days. My mom had been helping before Carey came down but my mom starts a new job today (Monday). At least her new job is really close to here so she can actually come by on her lunch breaks, which should help some.
Friday, June 30, 2006
Growing... and Shrinking Again
At my doctor's appointment yesterday, the doctor saw that my amniotic fluid levels were again far above normal. He went ahead and sent me next door to Bayfront for my third amnio reduction! I was actually glad because the fluid was starting to make me uncomfortable again and I would rather go in for the reduction before the excess fluid causes contractions.
They set me up in another broom closet sized room. (It turns out all their antepartum rooms are that small because those used to be their labor rooms before labor and delivery were combined in one room.) Carey and I thought to get before and after shots this time to show you all how I shrink down after the amnio reductions.
Dr. Prieto performed the amnio reduction again, removing 4.5 liters of fluid this time. It was even more uncomfortable than last time. After the procedure, I was in quite a bit of pain and the doctor explained that since my uterus has been expanding and contracting so much this pregnancy with the amniotic fluid changes, I was experiencing a muscle ache in the uterus. This made sense since it felt exactly like someone had stuck a booster shot or another shot to the muscle right into my belly! - Not pleasant. The doctor assisting Dr. Prieto, Dr. Needham, described it very well as a charley horse in the uterus.

All three doctors who were on the floor at the time of my amnio reduction were in the antepartum room with me but shortly after the procedure was finished, another patient came in with more urgent needs and they all left to attend her. Unfortunately, they left in such a rush, the nurse had to chase them down to get the order for pain killer (Toradol).

Shortly after they administered the Toradol, the uterus pain went away but I was having mild contractions. They gave me an extra dose of the Procardia and I waited for the go ahead to eat and drink, which I didn't get until around 9:00pm. They kept me overnight for observation to be sure that the contractions had stopped and discharged me this morning around 10:00am.
They set me up in another broom closet sized room. (It turns out all their antepartum rooms are that small because those used to be their labor rooms before labor and delivery were combined in one room.) Carey and I thought to get before and after shots this time to show you all how I shrink down after the amnio reductions.

Dr. Prieto performed the amnio reduction again, removing 4.5 liters of fluid this time. It was even more uncomfortable than last time. After the procedure, I was in quite a bit of pain and the doctor explained that since my uterus has been expanding and contracting so much this pregnancy with the amniotic fluid changes, I was experiencing a muscle ache in the uterus. This made sense since it felt exactly like someone had stuck a booster shot or another shot to the muscle right into my belly! - Not pleasant. The doctor assisting Dr. Prieto, Dr. Needham, described it very well as a charley horse in the uterus.

All three doctors who were on the floor at the time of my amnio reduction were in the antepartum room with me but shortly after the procedure was finished, another patient came in with more urgent needs and they all left to attend her. Unfortunately, they left in such a rush, the nurse had to chase them down to get the order for pain killer (Toradol).

Shortly after they administered the Toradol, the uterus pain went away but I was having mild contractions. They gave me an extra dose of the Procardia and I waited for the go ahead to eat and drink, which I didn't get until around 9:00pm. They kept me overnight for observation to be sure that the contractions had stopped and discharged me this morning around 10:00am.
Friday, June 23, 2006
Bed Rest
Just a couple weeks into bed rest and already sick of it.
I filled out an application online for temporary government assistance on Monday and was surprised to get a call back Tuesday from Kristy at the Department of Children & Families. They still needed some forms faxed to them (a copy of my medical insurance card, copies of Chris' pay stubs, a letter from my employer saying I am not working at this time and a doctor's note confirming that I am pregnant) but she said that we were eligible for food stamps and medicaid, though not for the cash assistance program. This should be very helpful during the time I am out of work and Kristy says that the medicaid will cover any expenses that my medical insurance does not (which could be anywhere around $1500.00 in co-pays and deductibles under our insurance plan) and will cover the twins' health care from birth up to a year.
 My mom came over every day last week to help out and has helped Hannah take an interest in potty training. I have been wanting to work with Hannah on potty training for some time now but have been unable to devote the time and energy necessary. Hannah has been keeping her diaper dry (except when asleep) for the most part and each time she uses the potty emerges from the bathroom with a victorious shout of "I did it!" and claps. At this rate, she will be completely potty trained very soon! I'm very proud of her.
My mom came over every day last week to help out and has helped Hannah take an interest in potty training. I have been wanting to work with Hannah on potty training for some time now but have been unable to devote the time and energy necessary. Hannah has been keeping her diaper dry (except when asleep) for the most part and each time she uses the potty emerges from the bathroom with a victorious shout of "I did it!" and claps. At this rate, she will be completely potty trained very soon! I'm very proud of her.
I received a call from HR and Benefits at Crum (where I work) and they ever so casually explained that since short term disability did not begin until July 1st and I have not been with the company a year yet, unless I returned to work before July 5th, they would start processing my termination. I was not happy about this news since I have enjoyed working there but had no options available. When Chris came home, though, he said that there had been a meeting at work (Chris works at the same place) and the big shots (including the owner of the company) were trying to find a way to help us out and from the sounds of it, did not want to lose me. It's still pretty much up in the air but I'm glad to know that there are those who are pulling for us at work.
I went in to my first appointment at the new OB's office last Thursday. There are three doctors at this office: Dr. Raimer, Dr. Montenegro and Dr. Prieto. I was feeling stretched almost to the limit again and was not exactly comfortable as I waited in the waiting room for almost an hour. Another woman in the waiting room says that this long of a wait is common. I spent the time talking to a new father of twins and a woman who is also expecting twin boys but was relieved when they finally called me back.
I saw Dr. Prieto and they did yet another ultrasound to check on the twins. Dr. Prieto said that my amniotic fluid levels were very high again but the fluid was now equal between the two twins and both twins were looking healthy. The doctor said that I still couldn't return to work and needed to schedule a routine fetal echo with All Children's Hospital's cardiologist, Dr. Huhta. He said this was just routine with any twin pregnancies. Dr. Prieto also said I need to come in weekly for ultrasounds from now on to keep a close eye on the amniotic fluid levels.
I had been experiencing itching in my hands and feet since my discharge from the hospital and the itching had spread to the rest of my body. When I had asked the nurse about it over the phone, she said I could take Benadryl for the itching but it hadn't been helping so I asked about the itching again. This time, they said that it might be a sign of a condition called Cholestasis so they gave me a scrip for blood work to test my bile acid levels and told me I had to fast from midnight before the blood work. I was eager to find out what was causing the itching and to make it stop so my mom looked up Cholestasis online as soon as we got home.
It sounded exactly like what I had so I decided to go for the blood work first thing in the morning. Unfortunately, I fell asleep pretty early in the afternoon and did not wake up again until after midnight so instead of fasting from midnight, I actually fasted from about 6:00pm so when I got to the lab, I was too light-headed for them to draw the blood (I almost passed out) so they told me I had fasted too long and to try again the next day (Saturday) at the one lab that was open on Saturdays. This time I made sure to eat something just before midnight and had no problem having the blood work done but I still had to wait for the results.
My sister, Carey, flew in to town around 11:00pm from Indiana with her kids and went to my parents house. The plan was that she would come over around 9:00am after dropping her kids off at her mother-in-law's.
However, late Saturday night I began feeling the tightness in my stomache that I had felt a couple of weeks before. I tried to just keep my feet up and relax, hoping it would subside and took my Procardia but the tightness continued and I woke Chris up at 4:00am on Father's Day to drive me to the hospital. I called the doctor and he said that he would inform the hospital that I was on my way and would most likely do another amnio-reduction. This actually sounded good to me because I remembered how much more comfortable I was after the first amnio-reduction and it hadn't been a painful experience.
When I got to the hospital, they set me up in a broom closet of a room. They had to move the bed in order to get the ultrasound equipment into the room! My dad and sister met us at the hospital and sat with us while we waited. I wasn't having very strong contractions according to the monitor and the nurse said that my cervix was closed but when the doctor arrived, he went ahead and ordered the amnio-reduction since the fluid levels were so high on both twins.


This time, the amnio-reduction was far from comfortable and I had to last through almost another 5 liters being withdrawn and this time they did a tap on each side to reduce fluid from each twin since the twins were even in their amounts of fluid. The doctor went ahead and ordered a chromosome analysis on the amniotic fluid from each side since they were removing the fluid anyway. The doctor said that I could most likely be discharged just a couple of hours later and I was happy to hear it, but shortly after the amnio-reduction, I started having rather intense and consistent contractions. The nurse checked my cervix again and said that I was dialated 2 cm so I was not going home that day.
They moved me to a regular labor/delivery room and started me on another medication to relax the uterus. I was still taking the Procardia but the Indomethacin can help stabilize the amniotic fluid as well as preventing contractions. They even put me back on the Magnesium Sulfate again. Shortly after they started the drip for the Magnesium Sulfate, the contractions stopped and things were looking better. My sister stayed with me at the hospital so Chris could go home and rest for work the next day.
The next afternoon, I was discharged after more ultrasounds since I was no longer contracting but they gave me a prescription to continue taking the Indomethacin for one more day and they told me to start taking the Procardia once every four hours instead of six. I was able to schedule the fetal echo at All Children's for Tuesday afternoon.
My friend, Lauren, came and picked up me, Carey and Hannah to go to my appointment Tuesday afternoon. It was a nice change getting to ride in a car with air conditioning. During my appointment (which ended up taking over two hours), Lauren and Carey took turns watching Hannah in the waiting room and sitting with me during the echo. It probably wouldn't have taken so long if the twins weren't so active. They kept dodging out of sight just when the tech was getting a good read on their heart.
Once Dr. Huhta had a chance to look at the results from the echo, he asked what prescriptions I was on and told me to stop the Indomethacin immediately - not to even take the one dose left. Turns out, Indomethacin can cause complications with the fetus heart and both twins were showing one chamber constricted. Dr. Huhta called Dr. Prieto's office to inform them that he was ordering me not to take the last dose of Indomethacin and had me schedule another echo for Thursday to verify that it was just the medication causing the problem.
Wednesday evening one of the ladies from our church came by with a delicious meal enough to feed all of us (me, Chris, Hannah, Carey and Caleb) and still have leftovers to eat the next night.
Yesterday (Thursday), as soon as my mom arrived to watch Hannah, my sister and I took off for All Children's for the follow-up echo. Dr. Huhta said that both hearts were looking much better now but they may schedule me for another echo later in the pregancy just to follow up. After the appointment at All Children's, Carey and I killed some time until my appointment at Dr. Prieto's office.
After yet another ultrasound, Dr. Prieto said that the twins look healthy and the fluid is even between the two twins and almost down to normal levels. I asked about the possibility of returning to work and he said that I can't yet but we'll see how I'm doing at next week's appointment.
They had the results back from the blood work and it confirmed that I do have Cholestasis so they gave me a prescription for Urso. He said that it's not a severe case and I should be fine since they'll be seeing me once a week anyway and can keep a close eye on my condition. Luckily, they say the only concern with this medicine is that it sometimes causes decrease of amniotic fluid so I shouldn't have any problems with this one. I'm looking forward to the itching stopping since it's been keeping me awake and driving me up the wall.
Who knows? Maybe I can make it to next Thursday's appointment without any trips to the hospital and maybe they'll let me return to work. This whole bed rest thing is not my cup of tea and is definitely making things tight financially.
I filled out an application online for temporary government assistance on Monday and was surprised to get a call back Tuesday from Kristy at the Department of Children & Families. They still needed some forms faxed to them (a copy of my medical insurance card, copies of Chris' pay stubs, a letter from my employer saying I am not working at this time and a doctor's note confirming that I am pregnant) but she said that we were eligible for food stamps and medicaid, though not for the cash assistance program. This should be very helpful during the time I am out of work and Kristy says that the medicaid will cover any expenses that my medical insurance does not (which could be anywhere around $1500.00 in co-pays and deductibles under our insurance plan) and will cover the twins' health care from birth up to a year.
 My mom came over every day last week to help out and has helped Hannah take an interest in potty training. I have been wanting to work with Hannah on potty training for some time now but have been unable to devote the time and energy necessary. Hannah has been keeping her diaper dry (except when asleep) for the most part and each time she uses the potty emerges from the bathroom with a victorious shout of "I did it!" and claps. At this rate, she will be completely potty trained very soon! I'm very proud of her.
My mom came over every day last week to help out and has helped Hannah take an interest in potty training. I have been wanting to work with Hannah on potty training for some time now but have been unable to devote the time and energy necessary. Hannah has been keeping her diaper dry (except when asleep) for the most part and each time she uses the potty emerges from the bathroom with a victorious shout of "I did it!" and claps. At this rate, she will be completely potty trained very soon! I'm very proud of her.I received a call from HR and Benefits at Crum (where I work) and they ever so casually explained that since short term disability did not begin until July 1st and I have not been with the company a year yet, unless I returned to work before July 5th, they would start processing my termination. I was not happy about this news since I have enjoyed working there but had no options available. When Chris came home, though, he said that there had been a meeting at work (Chris works at the same place) and the big shots (including the owner of the company) were trying to find a way to help us out and from the sounds of it, did not want to lose me. It's still pretty much up in the air but I'm glad to know that there are those who are pulling for us at work.
I went in to my first appointment at the new OB's office last Thursday. There are three doctors at this office: Dr. Raimer, Dr. Montenegro and Dr. Prieto. I was feeling stretched almost to the limit again and was not exactly comfortable as I waited in the waiting room for almost an hour. Another woman in the waiting room says that this long of a wait is common. I spent the time talking to a new father of twins and a woman who is also expecting twin boys but was relieved when they finally called me back.
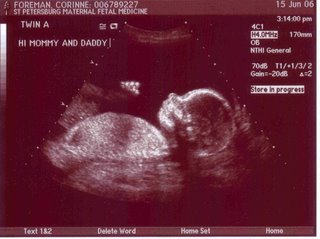
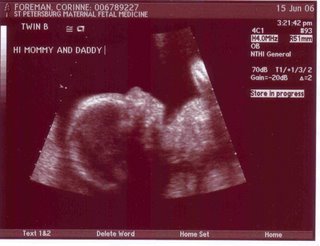
I saw Dr. Prieto and they did yet another ultrasound to check on the twins. Dr. Prieto said that my amniotic fluid levels were very high again but the fluid was now equal between the two twins and both twins were looking healthy. The doctor said that I still couldn't return to work and needed to schedule a routine fetal echo with All Children's Hospital's cardiologist, Dr. Huhta. He said this was just routine with any twin pregnancies. Dr. Prieto also said I need to come in weekly for ultrasounds from now on to keep a close eye on the amniotic fluid levels.
I had been experiencing itching in my hands and feet since my discharge from the hospital and the itching had spread to the rest of my body. When I had asked the nurse about it over the phone, she said I could take Benadryl for the itching but it hadn't been helping so I asked about the itching again. This time, they said that it might be a sign of a condition called Cholestasis so they gave me a scrip for blood work to test my bile acid levels and told me I had to fast from midnight before the blood work. I was eager to find out what was causing the itching and to make it stop so my mom looked up Cholestasis online as soon as we got home.
It sounded exactly like what I had so I decided to go for the blood work first thing in the morning. Unfortunately, I fell asleep pretty early in the afternoon and did not wake up again until after midnight so instead of fasting from midnight, I actually fasted from about 6:00pm so when I got to the lab, I was too light-headed for them to draw the blood (I almost passed out) so they told me I had fasted too long and to try again the next day (Saturday) at the one lab that was open on Saturdays. This time I made sure to eat something just before midnight and had no problem having the blood work done but I still had to wait for the results.
My sister, Carey, flew in to town around 11:00pm from Indiana with her kids and went to my parents house. The plan was that she would come over around 9:00am after dropping her kids off at her mother-in-law's.
However, late Saturday night I began feeling the tightness in my stomache that I had felt a couple of weeks before. I tried to just keep my feet up and relax, hoping it would subside and took my Procardia but the tightness continued and I woke Chris up at 4:00am on Father's Day to drive me to the hospital. I called the doctor and he said that he would inform the hospital that I was on my way and would most likely do another amnio-reduction. This actually sounded good to me because I remembered how much more comfortable I was after the first amnio-reduction and it hadn't been a painful experience.
When I got to the hospital, they set me up in a broom closet of a room. They had to move the bed in order to get the ultrasound equipment into the room! My dad and sister met us at the hospital and sat with us while we waited. I wasn't having very strong contractions according to the monitor and the nurse said that my cervix was closed but when the doctor arrived, he went ahead and ordered the amnio-reduction since the fluid levels were so high on both twins.


This time, the amnio-reduction was far from comfortable and I had to last through almost another 5 liters being withdrawn and this time they did a tap on each side to reduce fluid from each twin since the twins were even in their amounts of fluid. The doctor went ahead and ordered a chromosome analysis on the amniotic fluid from each side since they were removing the fluid anyway. The doctor said that I could most likely be discharged just a couple of hours later and I was happy to hear it, but shortly after the amnio-reduction, I started having rather intense and consistent contractions. The nurse checked my cervix again and said that I was dialated 2 cm so I was not going home that day.
They moved me to a regular labor/delivery room and started me on another medication to relax the uterus. I was still taking the Procardia but the Indomethacin can help stabilize the amniotic fluid as well as preventing contractions. They even put me back on the Magnesium Sulfate again. Shortly after they started the drip for the Magnesium Sulfate, the contractions stopped and things were looking better. My sister stayed with me at the hospital so Chris could go home and rest for work the next day.
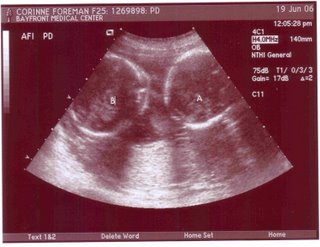
The next afternoon, I was discharged after more ultrasounds since I was no longer contracting but they gave me a prescription to continue taking the Indomethacin for one more day and they told me to start taking the Procardia once every four hours instead of six. I was able to schedule the fetal echo at All Children's for Tuesday afternoon.
My friend, Lauren, came and picked up me, Carey and Hannah to go to my appointment Tuesday afternoon. It was a nice change getting to ride in a car with air conditioning. During my appointment (which ended up taking over two hours), Lauren and Carey took turns watching Hannah in the waiting room and sitting with me during the echo. It probably wouldn't have taken so long if the twins weren't so active. They kept dodging out of sight just when the tech was getting a good read on their heart.
Once Dr. Huhta had a chance to look at the results from the echo, he asked what prescriptions I was on and told me to stop the Indomethacin immediately - not to even take the one dose left. Turns out, Indomethacin can cause complications with the fetus heart and both twins were showing one chamber constricted. Dr. Huhta called Dr. Prieto's office to inform them that he was ordering me not to take the last dose of Indomethacin and had me schedule another echo for Thursday to verify that it was just the medication causing the problem.
Wednesday evening one of the ladies from our church came by with a delicious meal enough to feed all of us (me, Chris, Hannah, Carey and Caleb) and still have leftovers to eat the next night.
Yesterday (Thursday), as soon as my mom arrived to watch Hannah, my sister and I took off for All Children's for the follow-up echo. Dr. Huhta said that both hearts were looking much better now but they may schedule me for another echo later in the pregancy just to follow up. After the appointment at All Children's, Carey and I killed some time until my appointment at Dr. Prieto's office.
After yet another ultrasound, Dr. Prieto said that the twins look healthy and the fluid is even between the two twins and almost down to normal levels. I asked about the possibility of returning to work and he said that I can't yet but we'll see how I'm doing at next week's appointment.
They had the results back from the blood work and it confirmed that I do have Cholestasis so they gave me a prescription for Urso. He said that it's not a severe case and I should be fine since they'll be seeing me once a week anyway and can keep a close eye on my condition. Luckily, they say the only concern with this medicine is that it sometimes causes decrease of amniotic fluid so I shouldn't have any problems with this one. I'm looking forward to the itching stopping since it's been keeping me awake and driving me up the wall.
Who knows? Maybe I can make it to next Thursday's appointment without any trips to the hospital and maybe they'll let me return to work. This whole bed rest thing is not my cup of tea and is definitely making things tight financially.
Monday, June 12, 2006
What a week!!!
Well, a lot has happened since Tuesday. Wednesday morning, I was feeling some tightness in the belly but figured I'd just mention it when I went in for my appointment at Dr. Igel's office. My mom picked me up and brought me to my doctor's appointment for 3pm. I was just meeting Dr. Igel's head midwife, Robyn Reese. Robyn was very optimistic during the beginning of the visit, saying how I could have her deliver the baby with Dr. Igel overseeing the birth and saying she didn't see any reason why I couldn't make it to term with the twins. Things changed, though, when she did the exam of my cervix. She basically said to forget everything she had just told me and to go directly from the doctor's office to the hospital. I was 1 centimeter dilated. She explained that there was low chance of survival for the twins if I delivered at 21 weeks and we needed to make sure I made it until at the very least 24 weeks.
My head was spinning as my mom drove me to the hospital. Chris got off work a little early to pick up Hannah and my dad and meet me and my mom at the hospital. While I checked in at Mease Countryside hospital, my mom and dad took Hannah back home with them.
The hospital set me up on IV with Magnesium Sulfate to stop the contractions. One of the nurses commented that I was laboring better than the laboring mothers. I was having strong, consistent contractions. After a while of the Magnesium Sulfate, they gave me a shot of muscle relaxer to assist the Magnesium Sulfate and an Ambien sleeping pill. They also did a bedside ultrasound, which showed that I had an abnormally high amount of amniotic fluid. The nurse said that the average count for amniotic fluid is between 5 and 20 but mine was at 60+! Before going to sleep, I heard the news report about a woman in Tampa who had been given an overdose of Magnesium Sulfate. It was not reassuring.
Chris' mom, Marcy, came to sit with me through the night so Chris could go home for a little bit and relieve my mom and dad. It was comforting to have Marcy with me since I was very uncomfortable and unsure of what was going to happen next.
Thursday morning I woke up still hazy from the Ambien to see Chris standing with Dr. Igel who explained that I was being transferred to Bayfront Hospital to Dr. Raimer's care. The doctor explained that the twins have Twin-to-Twin Transfusion Syndrome and what that means. I didn't really follow the explanation too well but I'm putting in a link to more information about this syndrome for you all to read. It all boiled down to: I needed to have an amnio-reduction done immediately.
While I was still half asleep, paramedics came in and transferred me from the hospital bed to a stretcher and transported me to Bayfront in a Critical Care Unit ambulance.
Shortly after arriving at Bayfront, my room was filled with doctors and interns and one doctor (who I later found out was Dr. Raimer) performed the amnio-reduction using an ultrasound to guide as they removed 5 liters of amniotic fluid from my abdomen! They kept offering painkillers but the procedure was virtually painless, though scary and bizarre.
Following the procedure, they kept me on IV and Magnesium Sulfate for a while and gave me a dose of Morphine to relax the uterus. They also gave me my Rhogam shot for my Rh negative blood type. Before long, the contractions had stopped entirely and I was feeling 100% better!
The doctors told me that it may be necessary to do another amnio-reduction or even transfer me to Tampa for a relatively new laser procedure but my ultrasound Friday morning showed great improvement and they took me off all the meds and even the IV. They had to keep me one more night for observation to be sure my amniotic fluids didn't build back up too quickly but Saturday morning the doctors said I was ready to go home... on bed rest. I have to take a medication called Procardia to keep my uterus relaxed and I have to schedule an appointment with Dr. Raimer's office for later this week.
I'm on bed rest pretty much until I deliver and apparently I will have to deliver at Bayfront (25 miles away from home) when the time comes. I am a little disappointed because I had heard rave reviews about Dr. Igel and the Mease Countryside facility and staff was very warm and comforting but Bayfront is better equipped for the possible complications that may arise and All Children's Hospital is right next door.
We appreciate all the thoughts and prayers that have gone out to us in this difficult time. We also greatly appreciate the offers for meals and help around the house. The journey's far from over. There's no telling how much longer until the twins deliver (the closer to 36 weeks, the better) and since I'm ordered on bed rest, we will have only one income for a while.
Please continue to pray for us as we still have numerous hurdles to jump. I will be calling around today to see if we can get on temporary WIC, CCC, etc. Hopefully we can get some assistance. We are going to need a new vehicle (preferably a minivan) before the twins come since our little Civic two-door won't fit two infant and one toddler car seats. We plan on trading in Chris' Mitsubishi truck but credit and down payment are still issues.
My head was spinning as my mom drove me to the hospital. Chris got off work a little early to pick up Hannah and my dad and meet me and my mom at the hospital. While I checked in at Mease Countryside hospital, my mom and dad took Hannah back home with them.
The hospital set me up on IV with Magnesium Sulfate to stop the contractions. One of the nurses commented that I was laboring better than the laboring mothers. I was having strong, consistent contractions. After a while of the Magnesium Sulfate, they gave me a shot of muscle relaxer to assist the Magnesium Sulfate and an Ambien sleeping pill. They also did a bedside ultrasound, which showed that I had an abnormally high amount of amniotic fluid. The nurse said that the average count for amniotic fluid is between 5 and 20 but mine was at 60+! Before going to sleep, I heard the news report about a woman in Tampa who had been given an overdose of Magnesium Sulfate. It was not reassuring.
Chris' mom, Marcy, came to sit with me through the night so Chris could go home for a little bit and relieve my mom and dad. It was comforting to have Marcy with me since I was very uncomfortable and unsure of what was going to happen next.
Thursday morning I woke up still hazy from the Ambien to see Chris standing with Dr. Igel who explained that I was being transferred to Bayfront Hospital to Dr. Raimer's care. The doctor explained that the twins have Twin-to-Twin Transfusion Syndrome and what that means. I didn't really follow the explanation too well but I'm putting in a link to more information about this syndrome for you all to read. It all boiled down to: I needed to have an amnio-reduction done immediately.
While I was still half asleep, paramedics came in and transferred me from the hospital bed to a stretcher and transported me to Bayfront in a Critical Care Unit ambulance.
Shortly after arriving at Bayfront, my room was filled with doctors and interns and one doctor (who I later found out was Dr. Raimer) performed the amnio-reduction using an ultrasound to guide as they removed 5 liters of amniotic fluid from my abdomen! They kept offering painkillers but the procedure was virtually painless, though scary and bizarre.
Following the procedure, they kept me on IV and Magnesium Sulfate for a while and gave me a dose of Morphine to relax the uterus. They also gave me my Rhogam shot for my Rh negative blood type. Before long, the contractions had stopped entirely and I was feeling 100% better!
The doctors told me that it may be necessary to do another amnio-reduction or even transfer me to Tampa for a relatively new laser procedure but my ultrasound Friday morning showed great improvement and they took me off all the meds and even the IV. They had to keep me one more night for observation to be sure my amniotic fluids didn't build back up too quickly but Saturday morning the doctors said I was ready to go home... on bed rest. I have to take a medication called Procardia to keep my uterus relaxed and I have to schedule an appointment with Dr. Raimer's office for later this week.
I'm on bed rest pretty much until I deliver and apparently I will have to deliver at Bayfront (25 miles away from home) when the time comes. I am a little disappointed because I had heard rave reviews about Dr. Igel and the Mease Countryside facility and staff was very warm and comforting but Bayfront is better equipped for the possible complications that may arise and All Children's Hospital is right next door.
We appreciate all the thoughts and prayers that have gone out to us in this difficult time. We also greatly appreciate the offers for meals and help around the house. The journey's far from over. There's no telling how much longer until the twins deliver (the closer to 36 weeks, the better) and since I'm ordered on bed rest, we will have only one income for a while.
Please continue to pray for us as we still have numerous hurdles to jump. I will be calling around today to see if we can get on temporary WIC, CCC, etc. Hopefully we can get some assistance. We are going to need a new vehicle (preferably a minivan) before the twins come since our little Civic two-door won't fit two infant and one toddler car seats. We plan on trading in Chris' Mitsubishi truck but credit and down payment are still issues.
Tuesday, June 06, 2006
Mommy's 25th Birthday
Yesterday was my 25th birthday and one I will not likely forget soon...
First, Sunday morning we awoke to find that our car had been stolen from our condo parking lot... Chris and I had planned on a fun afternoon with friends by the pool that day so after reporting the car stolen to the police and insurance company, we went on with those plans. There was nothing to do but wait and hope they found the car. We now know the importance of theft coverage on the insurance too little too late.
Luckily, around 4:00 we got a call from the police department that they had found the car... unfortunately, it was found without any wheels. The thieves dumped our car in Pinellas Park, taking with them all four wheels, the spare tire, the tire jack, my access badge from work and a large box of diapers for Hannah that we had bought Saturday night! They had also clearly rifled through our glove compartment. An information card with our bank account numbers and routing number was sitting on the passenger seat.
The next morning, we crammed into Chris' truck (not exactly a vehicle built for three) and Chris dropped me off at work and Hannah off at daycare before running around all over town to get new wheels for the car and change our bank account number.
Overall, my birthday was looking up later in the day. My co-workers decorated my cubicle at work, we had a large strawberry cake and ordered pizza for lunch. After work, my friend Lauren picked me up from work and Hannah up from daycare and we went to the mall to spend the gift card she had given me for Motherhood. Once we were all shopped out, we met Chris at Olive Garden for dinner. Chris had gotten the wheels and we had use of the car again.
Later last night, though, I started feeling sharp, uncomfortable tightness in the belly that was making it impossible to sleep. Chris insisted I call the midwife for advice. We've been seeing Gina Tregellis, head midwife at Countryside Birthing Place but are scheduled to meet Dr. Stephen Igel (OB/Gyn) and his head midwife, Robin, this Wednesday (tomorrow) at 3:00. I called Gina and she told me that we should go to the hospital just to be on the safe side. We woke Hannah up and headed for the hospital. I was afraid I might just be over-reacting and was depriving us all of sleep for nothing but when we got to Mease Countryside Hospital, they hooked me up to a contraction monitor and found that I was having small contractions. I almost felt relieved to hear it. At least I knew that I wasn't over-reacting to nothing.
The nurse gave me a shot of a medication called Terbutaline ("Terb") to relax the uterus. She gave me a small dose to see how I reacted and it was a good thing because my blood pressure shot up and my pulse slowed down and I got very light-headed. They decided to give me fluids via IV to hydrate me instead of giving me more Terb. I then waited for the ultrasound tech to arrive so that they could get an accurate heart rate on each of the twins. (The doppler had picked up a lot of noise from all their moving around but they could get a clear heart rate for either twin.)
The ultrasound tech was very patient with me while I kept having to roll onto my side because lying on my back made me light-headed and nauseous. Chris got to see the ultrasound this time and one baby was still being more aggressive. While one baby was curled up, the other rested his legs on top of his brother. I'm glad to report that both babies are still healthy and active with good heart rates.
Once I was hydrated with the IV and the contractions had stopped, they gave me the okay to leave but said that Dr. Igel's midwife, Robin, had ordered that I stay home and rest until the appointment on Wednesday as a precaution. At least the appointment's not far in the future. When we returned home, I fell right to sleep and had the most comfortable sleep I've had in weeks!
I hope to return to work on Thursday but my work says that I need a doctor's note stating that it's okay for me to return to work.
Keep us in your prayers... especially Wednesday.
First, Sunday morning we awoke to find that our car had been stolen from our condo parking lot... Chris and I had planned on a fun afternoon with friends by the pool that day so after reporting the car stolen to the police and insurance company, we went on with those plans. There was nothing to do but wait and hope they found the car. We now know the importance of theft coverage on the insurance too little too late.
Luckily, around 4:00 we got a call from the police department that they had found the car... unfortunately, it was found without any wheels. The thieves dumped our car in Pinellas Park, taking with them all four wheels, the spare tire, the tire jack, my access badge from work and a large box of diapers for Hannah that we had bought Saturday night! They had also clearly rifled through our glove compartment. An information card with our bank account numbers and routing number was sitting on the passenger seat.
The next morning, we crammed into Chris' truck (not exactly a vehicle built for three) and Chris dropped me off at work and Hannah off at daycare before running around all over town to get new wheels for the car and change our bank account number.
Overall, my birthday was looking up later in the day. My co-workers decorated my cubicle at work, we had a large strawberry cake and ordered pizza for lunch. After work, my friend Lauren picked me up from work and Hannah up from daycare and we went to the mall to spend the gift card she had given me for Motherhood. Once we were all shopped out, we met Chris at Olive Garden for dinner. Chris had gotten the wheels and we had use of the car again.
Later last night, though, I started feeling sharp, uncomfortable tightness in the belly that was making it impossible to sleep. Chris insisted I call the midwife for advice. We've been seeing Gina Tregellis, head midwife at Countryside Birthing Place but are scheduled to meet Dr. Stephen Igel (OB/Gyn) and his head midwife, Robin, this Wednesday (tomorrow) at 3:00. I called Gina and she told me that we should go to the hospital just to be on the safe side. We woke Hannah up and headed for the hospital. I was afraid I might just be over-reacting and was depriving us all of sleep for nothing but when we got to Mease Countryside Hospital, they hooked me up to a contraction monitor and found that I was having small contractions. I almost felt relieved to hear it. At least I knew that I wasn't over-reacting to nothing.
The nurse gave me a shot of a medication called Terbutaline ("Terb") to relax the uterus. She gave me a small dose to see how I reacted and it was a good thing because my blood pressure shot up and my pulse slowed down and I got very light-headed. They decided to give me fluids via IV to hydrate me instead of giving me more Terb. I then waited for the ultrasound tech to arrive so that they could get an accurate heart rate on each of the twins. (The doppler had picked up a lot of noise from all their moving around but they could get a clear heart rate for either twin.)
The ultrasound tech was very patient with me while I kept having to roll onto my side because lying on my back made me light-headed and nauseous. Chris got to see the ultrasound this time and one baby was still being more aggressive. While one baby was curled up, the other rested his legs on top of his brother. I'm glad to report that both babies are still healthy and active with good heart rates.
Once I was hydrated with the IV and the contractions had stopped, they gave me the okay to leave but said that Dr. Igel's midwife, Robin, had ordered that I stay home and rest until the appointment on Wednesday as a precaution. At least the appointment's not far in the future. When we returned home, I fell right to sleep and had the most comfortable sleep I've had in weeks!
I hope to return to work on Thursday but my work says that I need a doctor's note stating that it's okay for me to return to work.
Keep us in your prayers... especially Wednesday.
Sunday, May 21, 2006
Monday, May 15, 2006
Still Growing...

Only a week since the last post and Mommy's belly has gotten even larger!!!
Co-workers are commenting every day that my belly's bigger than the day before. My next prenatal checkup is May 26th. Shortly after that appointment the midwife will have to transfer care to an OB doctor. Multiples pregnancies are considered high risk in America and so twin births are restricted to hospitals with obstetric doctors and water birth is out of the question. I'm very disappointed, as Chris and I were looking forward to a water birth in a birthing center with minimal intervention. We can only hope and pray now that we can find an obstetric doctor who sympathizes with our wishes to have as natural a birth as possible without endagering the babies or myself. I strongly believe that childbirth is a natural event and wish to avoid cesarean. Please keep us in your prayers as we search for an obstetric doctor.
Saturday, May 06, 2006
Growing Mommy!
Subscribe to:
Posts (Atom)